Vector Borne Diseases (VBDs) are caused by parasites, viruses and bacteria, which threaten the human health by causing infection. Mosquitoes, sandflies, bugs, ticks, mites and others transmit these diseases. The National Vector Borne Disease Control Programme (NVBDCP) under Ministry of Health and Family Welfare, Government of India, addresses six VBDs-Malaria, Lymphatic Filariasis (LF), Dengue, Chikungunya, Japanese Encephalitis (JE) and Kala-azar (KA). Three diseases; Kala-azar, Lymphatic Filariasis& Malaria are under elimination by 2030 as per Sustainable Development Goals (SDGs).
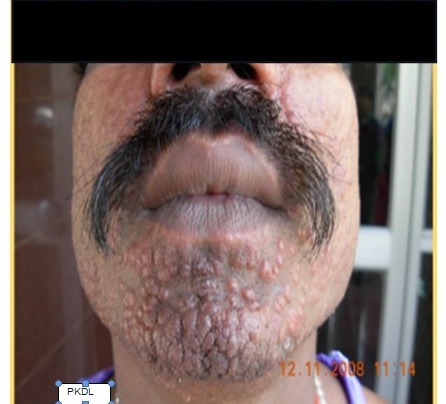
Kala-azar, also known as visceral leishmaniasis, is a severe parasitic disease transmitted by the bite of infected female Phlebotomusargentipes (sandfly). Kala-azar causes prolonged irregular fever (>2 weeks), anaemia, enlarged spleen (splenomegaly), weight loss, loss of appetite, weakness and sometimes darkened skin (for which the disease is called kala-azar or black fever).Post-kala-azar dermal leishmaniasis (PKDL) is a non-lethal complication of kala-azar that can develop months or years after treatment. PKDL can appear as a macular, papular, or nodular rash, and it usually starts on the face but can spread to other parts of the body. In 1920, Dr.UpendranathBrahmachari discovered urea stibamine, which is the urea salt of para-amino phenyl stibnic acid and it revolutionized the treatment of Kala-azar with >90% cure rate and with minimal side effects. This discovery of Dr.Brahamachari, then professor of Tropical Diseases at Campbell Medical College, Calcutta (presently known as NilratanSircar Medical College) had a significant impact on public health, saving countless lives in India and beyond. He is also credited with the description of PKDL. The Government of India launched the National Kala-azar Elimination Programme in 1991-1992 with a target to reduce the number of cases and deaths from kala-azar. The program was included under NVBDCP in 2003. As per SDG, the KA is supposed to be eliminated by 2030 in all the WHO member countries including India. Efforts to eliminate Kala-azar from India have been an ongoing process since 2003. However, India achieved target of elimination as public health problem in 2023. The target of elimination was achieved by India as per WHO criteria of annual incidence of <1 case per 10,000 population at the sub-district level (block level). For getting WHO certification, elimination level needs to be sustained for a period of three years, up to 2026.
Kala-azar or Visceral Leishmaniasis is endemic in 80 countries of the World and 5% (599) of kala-azar cases reported by India vs global cases (11762) in 2023
This goal has been largely achieved in many endemic districts in India, especially in 4 States of Bihar, Jharkhand, West Bengal, and Uttar Pradesh, which had the highest case burden historically. However, more than 90% of kala-azar cases are contributed by Bihar and Jharkhand only. The disease is endemic in 633 blocks of 54 districts in the 4 States as mentioned above, out of which 458 blocks (72%) belong to only Bihar. According to recent data, all the affected blocks except one have achieved the target of elimination even below level 0.5 per 10,000 population.
The kala-azar Elimination Programme Strategies being followed in India as below:
Early Diagnosis & Complete Case Management
- Active Case Search (ACS) four times in a year
- Initiation of treatment within 3 days
- Periodic follow up of KA and PKDL cases (15/30/180/365 day in first year and thereafter once for two years)
- Engagement of Rural Health Practitioners, PRI members, SHGs etc
Integrated Vector Control & Vector Surveillance
- 2 times Indoor Residual Spray (IRS) with synthetic pyrethroid and use of hand compression pump in all endemic villages with Active Case Search
- Focal IRS spray in new village of Kala-azar reported case
- Pre and Post vector surveillance after IRS
Supervision, Monitoring, Surveillance & Evaluation
- Real time reporting of cases in Kala-azar Management Information System (KAMIS) & would likely to be in the domain of integrated Health Information Platform (IHIP) shortly
- Periodic monitoring and reviews by District Magistrates/Block officers and State officials
- Periodic programme review by Central team during active case search and IRS activities
Engagement of Rural Health Practitioners, PRI members, SHGs etc.
- Asymptomatic Carriers: Some people carry the parasite without showing symptoms, making it hard to detect and control all sources of infection.
- Relapse Cases: Even when patients are treated, relapses can occur, potentially reintroducing the infection into areas.
- Sandfly Control: Sandfly prefers dark, shady, damp areas, is poor flier moving in short hopping flights and can hop up to 6 feet. The Sandflies favours resting sites of soil cracks and crevices (especially in mud hut), burrows of rodents, tree holes, termite hills, caves, bird tunnel, earthen mounds, under stone and foliage, etc. and also thrive in poor living conditions, making it essential to improve housing and sanitation in affected areas.
- Climate and Socioeconomic Factors: These factors affect sandfly populations and disease transmission, making control efforts more challenging.
Therefore, the engagement of local community (Rural Health Practitioners, PRI members, SHGs etc.) is very vital for awareness of the KA programme and implementation of different activities at the grass-root level.
Approaches and Next Steps
- Intensified Surveillance and Vector Control: Targeting residual sandfly populations and tracking cases more closely is key to sustaining control.
- Improved Diagnostics and Treatment Access: Faster diagnostics and broader access to effective treatment like miltefosine, amphotericin B, and paromomycin have been instrumental. However, introduction of single day single dose injection of Liposomal Amphotericin B (LAmB) in 2015, instead of 28 days treatment with miltefosine is one of the landmark decision of the programme.
- Community Engagement: Educating and involving local communities can help ensure that cases are detected early, and transmission is limited.
- Engagement of 22 Medical Colleges in 4 states in 2022 to enhance surveillance and service delivery for kala-azar affected patients.
Prospects for Elimination
- With sustained efforts, experts are optimistic that India can sustain the elimination level of Kala-azar<1/10000 population in next two years and get elimination certificate of kala-azar from WHO in due time before 2030. The key is to maintain the current momentum, address existing challenges, and ensure high coverage in areas where cases persist.
The WHO and Indian government remain committed to full elimination and certification by 2026 or thereafter but before 2030 with sustained and targeted efforts.
Dr.Sudarsan Mandal, Sr. CMO, NCVBDC & Formerly DDG (TB/NCD/Leprosy), Dte.GHS, MoH&FW
Dr Ashish Bhat is a Doctoral Scholar in Health Systems and Policy at the School of Health Systems, Tata Institute of Social Sciences, Mumbai